Beyond Calories: What Refeeding Syndrome Teaches Us About Nutrition and Resilience
- Healing_ Passion
- Sep 27, 2025
- 3 min read
Updated: Oct 8, 2025
When most people think about nutrition, one word comes to mind: calories.
For decades, medical and dietary advice has been shaped by the idea that “too many calories” cause obesity and that “more calories” are the cure for malnutrition.
But what if this view misses the deeper truth of how our bodies actually work?
One of the clearest examples comes from a condition known as refeeding syndrome.
What Is Refeeding Syndrome?
Refeeding syndrome (RS) occurs when calories are suddenly reintroduced after a period of starvation or severe undernutrition. At first, giving food or intravenous nutrition seems like the right step. But in RS, those calories can trigger a dangerous chain reaction:
Insulin surges as glucose enters the bloodstream.
Electrolytes like phosphorus, potassium, and magnesium shift rapidly into cells, leaving blood levels dangerously low.
Thiamin (vitamin B1), essential for burning glucose, gets depleted.
The result: arrhythmias, organ failure, even death if not recognized early.
In short: calories without nutrient support can collapse the system.
The Other Edge: Obesity and the Calorie-Centric Paradigm
At the opposite extreme is obesity. For decades, obesity has been described in simple calorie terms: “too much energy in, not enough energy out.” This lens has dominated nutritional practice, policy, and public health campaigns.
But just as with RS, this view falls short. Excess calories without nutrient balance create their own form of metabolic instability:
Insulin resistance
Lipotoxicity and ectopic fat accumulation
Chronic low-grade inflammation
Accelerated wear on systems of repair and resilience
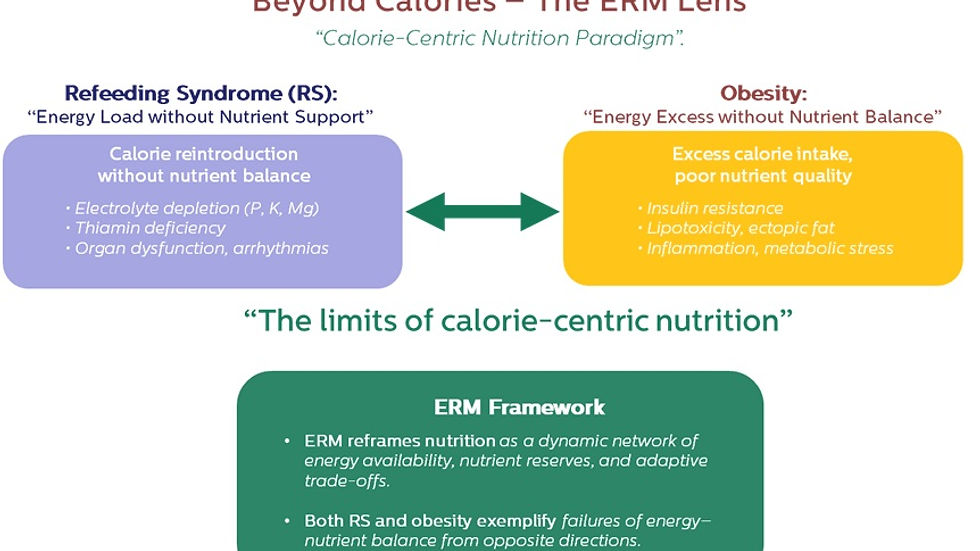
So whether it’s too many calories (obesity) or calories without nutrient reserves (RS), both reveal the same truth: nutrition is not just about calories.
Enter the ERM Framework
This is where the concept of Exposure-Related Malnutrition (ERM) offers a new perspective. ERM reframes nutrition as a dynamic network of energy availability, nutrient reserves, and adaptive trade-offs.
In RS, energy is reintroduced without the buffer of nutrient reserves → collapse.
In obesity, energy is in chronic excess without resolution or nutrient balance → maladaptation.
In ERM, the focus shifts to how well the body can allocate, balance, and resolve its energy–nutrient trade-offs under stress, aging, and chronic disease.
ERM shows us that resilience depends on more than just energy supply. It depends on how energy and nutrients work together to support recovery, repair, and long-term stability.
Why This Matters
For clinicians: It’s not enough to count calories. Screening for nutrient reserves, electrolyte status, and adaptive capacity is essential.
For individuals: Eating isn’t just fueling — it’s building resilience. Quality, timing, and context matter as much as quantity.
For public health: Moving beyond calorie-centric policies could transform how we approach obesity, malnutrition, and chronic disease prevention.
The Path Forward
Understanding nutrition through the lens of ERM opens up new possibilities. It encourages us to think beyond mere numbers. We must consider how our bodies interact with food.
What if we focused on nutrient density instead of calorie counts? Imagine a world where we prioritize foods rich in vitamins and minerals. This shift could lead to better health outcomes.
Conclusion
Refeeding syndrome and obesity might seem like opposites, but they both prove the same point: calories alone do not define nutrition.
The ERM framework helps us see nutrition not as a math equation of energy, but as a living system of balance, adaptation, and resilience. By embracing this perspective, we can foster a deeper understanding of our health and well-being.
Takeaway: Nutrition is a complex interplay of energy and nutrients. Let’s move forward with a holistic view that promotes health and vitality.
da Silva, J. S. V., Seres, D. S., Sabino, K., Adams, S. C., Berdahl, G. J., Citty, S. W., Cober, M. P., Evans, D. C., Greaves, J. R., Gura, K. M., Michalski, A., Plogsted, S., Sacks, G. S., Tucker, A. M., Worthington, P., Walker, R. N., Ayers, P., & Parenteral Nutrition Safety and Clinical Practice Committees, American Society for Parenteral and Enteral Nutrition. (2020). ASPEN consensus recommendations for refeeding syndrome. Nutrition in Clinical Practice, 35(2), 178–195. https://doi.org/10.1002/ncp.10474
Refeeding syndrome, Electrolyte imbalance, Malnutrition, Nutrition support, ASPEN consensus




Comments